(Un)Fair Care
How Emersonians are working to make healthcare more equitable and accessible for all
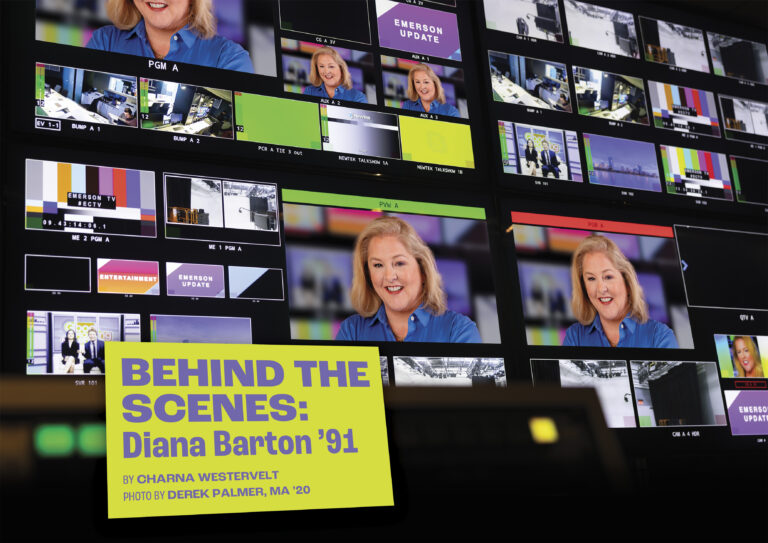
Cover photo by Derek Palmer
In the 1980s, when Philip Finch, MA ’97, visited his doctor at Fenway Health in Boston, he watched as fellow patients slipped into the Fenway neighborhood building through an unmarked door in a back alley.
Some patients of the then small center, which provided care for a number of gay and lesbian residents in the neighborhood, feared they would be taunted, or worse yet, that they would be victims of an attack. Back then, it wasn’t uncommon for gay men and women who needed healthcare, but were afraid of discrimination, to delay seeing a doctor, or even go without. In 1981, Fenway Health made the first diagnosis of HIV/AIDS in New England.

“At the time, you didn’t want to be identified with walking into a gay health center,” said Finch, a graduate of the Global Marketing/Communications program who identifies as gay. “It’s hard to believe society was that way.”
Fast forward four decades, and Fenway Health—where Finch spent 15 years of his career as a communications professional—now finds itself in a modern, 10-story, 100,000-square-foot facility. It’s the largest building ever constructed by an organization with a mission to serve the LGBTQIA+ community. These days, patients proudly walk through the front door.
Yet, despite the progress in the US toward improving access to high-quality healthcare for all people, major barriers remain. A transgender patient skips a mammogram because a technician might do a double take when their appearance and name don’t match their anatomy. A Black woman won’t get pregnant because she knows she’s more likely to die from pregnancy complications than her White friends. In a rural area, a Native American teen with a heart problem deteriorates when his family can’t afford to send him to a larger city for care.
Over the last nine months, the COVID-19 pandemic and Black Lives Matter protests held across the country have propelled these disparities even more into the spotlight. Research has shown that racial and ethnic minorities are disproportionately affected by COVID-19. Coronavirus hospitalization rates among non-Hispanic Black people and Hispanic or Latino people were both nearly five times the rate of non-Hispanic Whites, according to recent data from the Centers for Disease Control and Prevention.
“If we want people to adopt healthier behaviors, we have to make healthier places to live and work. And where we can’t do that, we at least have to acknowledge how our communities directly influence our health.”
Andrea Mooney ’08, director of health communications, Bureau of Community Health and Prevention, Massachusetts Department of Public Health
At the same time, violence against Black people, at the hand of the police and others, and the ensuing nationwide protests, have highlighted the persistence of racial injustice and inequities, institutional racism, and structural violence in the US—problems that have also permeated the healthcare system.
In response, Emerson alumni in the field have redoubled their efforts to work toward equitable access to healthcare for all. Finch, Andrea Mooney ’08, and Shanaé Burch ’13 are setting their sights on a time when all people in the US can easily access high-quality, affordable healthcare with no roadblocks.
Creating a Welcoming Environment
After graduating from Cornell University with a degree in history and government, Finch moved to Boston, where he worked for 10 years in marketing communications in financial services. He also became a patient at Fenway Health, volunteered there, and was drawn to the organization. “I really connected with their mission,” he said.
Looking for formal communications training, in the mid-1990s, Finch applied to Emerson and was accepted into the school’s Global Marketing/Communications program, which at the time was based in Belgium. Finch packed up again and moved overseas.
The program, he says, helped him understand the importance of considering a wide variety of perspectives when communicating. He recalls a class project during which he and his classmates helped launch the same business in three different countries, taking into account language and cultural differences. “I learned that there’s not just one way of doing things,” he said.
After graduation, Finch consulted for a few years before a communications position opened at Fenway Health. He threw his name in the hat and got the job. He was proud of the center’s history of providing compassionate care for gay men suffering from AIDS in the 1980s, and he wanted to help further its mission.
At Fenway, Finch led internal and external communications, served as a spokesperson, and oversaw the center’s $15 million capital campaign for a new building project, the 100,000-square-foot facility that opened in 2009.
“A great way to help fight health disparities is to create a welcoming environment for people,” he said. “The building is a monument to the LGBTQIA+ community.”
Over the years, Finch has helped lead Fenway Health in crafting its message as it became a magnet for LGBTQIA+ patients across New England seeking compassionate, professional care. Patients, in fact, were driving to the center from as far away as rural Vermont and Maine to receive healthcare.
“That was great,” Finch said. “But there should have been a place where they felt safe getting care in Maine and Vermont.”
He knows that there is still a lot of work to be done to make healthcare accessible to all. Even when safe places for care do exist for LGBTQIA+ populations, the issues persist.
For example, lesbians, who may be at a higher risk for breast cancer and need to be screened differently, may not receive the best care if they feel uncomfortable discussing their sexual orientation.
Many transgender people are also reluctant to go to the doctor, said Finch. “Even if the provider wants to do the right thing, their reaction [to realizing a patient is transgender] can make [the patient] feel ashamed. So, many transgender people go to the doctor less.” Accessing compassionate healthcare can be even more of a challenge for LGBTQIA+ people of color, he said.
To help address that issue, Fenway collaborated with other community organizations to better understand the cultural and acceptance differences in LGBTQIA+ communities of color, later creating safe spaces in areas where people were more likely to access care and developing a targeted messaging strategy to help get the word out.
Now, as a consultant, Finch works with health centers and health facilities on projects such as creating spaces that are more welcoming and inviting for all patients, or making intake forms more inclusive by providing sections for both “preferred name” and “legal name.”
“It makes it really tough for a person to feel comfortable if, when they see a doctor, the doctor says, ‘I thought I was seeing David, not Sarah.’” Then, Finch helps the organization craft a plan on how to communicate the changes to staff and patients.
During the coronavirus pandemic, Finch has been disheartened to see certain communities in the US suffering more than others. “The people impacted the most are typically marginalized,” he said. “They have front-line service jobs and less opportunity to work remotely. They may not be eligible for sick leave or other benefits. They may not even want to know what their COVID situation is, because if they’re positive, they need to quarantine, and many people can’t afford to take two weeks off.”
He believes a major hurdle in the US is the lack of a national sick leave policy. That’s been problematic during the COVID-19 pandemic and has likely been a factor in community spread of the virus. But it’s also a problem during non-pandemic times. Without adequate sick days, many workers don’t have enough time to recover from illness, and that negatively impacts their overall health. Preventative care can also fall by the wayside.
Finch is optimistic that positive change will ultimately emerge from the pandemic. “There will be silver linings,” he said. “The next decade, especially, will be telling for the future of healthcare in the US.”
Racial Equity During a Pandemic
Andrea Mooney ’08 had a different challenge on her hands last March. As the full scope of the global pandemic came into clear view, Mooney and her team at the Massachusetts Department of Public Health’s Bureau of Community Health and Prevention raced to design and launch campaigns to educate the public not only about the coronavirus and how to stay safe, but also about how equity plays a role in health outcomes.
More than anything, Mooney, who is the Bureau’s director of health communications, wanted to frame the campaigns within a racial equity lens, acknowledging the root causes of health inequities and the multiple barriers that get in the way of people’s access to better healthcare.
“Artists and cultural workers have a responsibility and an innate intuition to imagine what change could look like.”
Shanaé Burch ’13, doctoral student at Teachers College at Columbia University
“If we want people to adopt healthier behaviors, we have to make healthier places to live and work,” she said. “And where we can’t do that, we at least have to acknowledge how our communities directly influence our health.”
One fact sheet that she and her team created, on chronic diseases and COVID-19, immediately acknowledged these disparities and their causes. “COVID-19 has further exacerbated the historical and current inequities in our society,” the sheet says. It goes on to explain how people of color are at a higher risk for chronic diseases due to health consequences of structural racism, which increases their risk for serious complications from COVID-19.
“It’s not because of individual behaviors or coincidence,” Mooney said. “It’s decades and centuries of oppression and racism.”
The fact sheet also purposefully includes compassionate language. Stay home “when you can,” it says, a nod to essential workers who might not be able to shelter in place. “We wanted to acknowledge all of the barriers and community factors that play a part in people’s lives,” Mooney said.
Mooney is a firm believer that the key to lasting change when it comes to improving health outcomes is to focus on improving community conditions and not just individual behaviors. “Many people think living conditions are indirect factors,” she said. “But, in fact, they make up most of our health. It’s on us as public health practitioners to help improve access to healthy options in these communities.”

But it’s not just public health practitioners. Educators, city planners, employment lawyers, and others working in the “social determinants of health” sphere all need to scrutinize their industry to see how it’s affecting the health and wellness of their community, Mooney said.
“We have to genuinely collaborate with communities,” she said. “We have to lift up community voices and put them central in everything we do, without causing additional burden.”
In many ways, Mooney is doing the work she set out to do when she was at Emerson. A Writing, Literature and Publishing major, she wanted to use communication to create a better world but wasn’t quite sure how to do it. Her courses helped expand her worldview. “In every class, whether it was fiction or advocacy or globalization, we were encouraged to look at all sides.”
After graduating, she covered the 2008 Summer Olympics in Beijing as a journalist, worked at a travel media company, and was then a senior writer at Boston Children’s Hospital. In 2015, she earned a Master of Public Health from George Washington University and later worked in communications at a global health agency and a US-based social marketing firm before starting her current job.
Now, in her role at the Massachusetts Department of Public Health, Mooney keeps racial equity top-of-mind as she works to improve the health and well-being of everyone in the state. She’s hopeful the US will start to move toward meaningful change.
Throughout the country, “there is so much to fix,” Mooney said, “but nowhere does it say that one person has to fix everything. People are problem-oriented, but we need to be solution-oriented. We need to ask ourselves, what can I do in my little sphere of influence?”
The Influence of the Arts
Meanwhile, in New York City, Shanaé Burch ’13 is asking, and answering, that very question. As a fourth-year doctoral student in health education at Teachers College at Columbia University, she is studying how arts participation and creativity impact health outcomes. Current interests include how to support theater companies in transforming themselves into becoming more proactive about public health needs, and how creativity can influence health consciousness.

“The arts and culture sector is being tapped to address public health issues,” Burch said. “Artists and cultural workers have a responsibility and an innate intuition to imagine what change could look like.”
Burch, who also is a Health Policy Research Scholar at the Robert Wood Johnson Foundation, took an unconventional path to pursuing her passion for health literacy and activism.
After graduating from Emerson with a degree in Acting, Burch worked as a professional actor, appearing in stage productions across Boston. She also earned an EdM in Arts in Education from the Harvard Graduate School of Education.
In recent years, she played the part of Keera in the Huntington Theatre’s production of Milk Like Sugar, written by playwright and former adjunct Emerson professor Kirsten Greenidge. The play tackled the topic of teen pregnancy.
But even as Burch enjoyed a successful acting career, she saw firsthand how grueling workweeks—with late nights and little time off, especially leading up to productions—made it harder for people with chronic illness or disabilities, she said.
She vividly recalls an Emerson course that piqued her interest in healthcare early on. During a health communication class her senior year, she was engrossed in a documentary about whether inequities were making Americans sick.
“It was in that course that I realized, no matter my level of education, no matter my ZIP code, as a Black woman I’m more likely to lose a child during its first year of life or die during childbirth than a White woman with a high school diploma. It set me on a journey.”
At the Robert Wood Johnson Foundation, Burch is one of several dozen scholars from underrepresented communities in the leadership program. She participates in policy and leadership development trainings and coursework, receives health equity training, and connects with public health and policy leaders.
“It’s helping me make connections between my research and policy change,” she said.
In one project, Burch and a group of fellow scholars evaluated language in the CARES Act regarding recovery and support services for those addicted to opioids and made recommendations that would make funding more equitable.
As a Board Member of the Black Caucus of Health Workers (BCHW)—the American Public Health Association’s oldest caucus—Burch is currently working on an oral history storytelling project, interviewing the group’s Black public health leaders about their work. Recently over Zoom, she spoke with BCHW co-founder Dr. June Jackson Christmas, the first African American woman president of the American Public Health Association. Ultimately, Burch and other volunteers will build a video library and produce a mini-documentary highlighting a selection of interviews.
“We hope that by sharing her story and other stories, we’ll remain hope-filled with the affirmation that our Black Lives Matter,” Burch says. “Our research focuses, specialties, and stories as Black public health professionals matter.”
Burch has visions of herself post-graduation working at a center that meshes arts and public health. Indeed, increasingly, art is being prescribed by physicians as therapy. Through a program in Massachusetts, for example, admission to arts and cultural organizations are heavily discounted for those who receive health insurance through the Commonwealth’s ConnectorCare program, which is available to lower-income residents. In Montreal, patients with physician prescriptions for a museum visit get in to the Montreal Museum of Fine Arts for free, while research from the UK found that joining a choir can boost one’s mental health.
“In a dream world, I play matchmaker and curator,” Burch said. “I’d pair artists and academics and public health folks to design creative, imaginative experiences. We’d increase health literacy, amplify community wealth and knowledge, and get us all closer to living a healthier life.”
Finch is similarly hopeful. “We have the resources, the intelligence, and the research to provide the best care in the world for every person in our country,” he said. “I hope that we do that.”